As the world begins to re-open with the COVID-19 pandemic, detecting new outbreaks has rapidly become a major policy challenge. As the disease prevalence increases in certain areas, we’ve seen policymakers fall back and return to a less-open state of affairs. The problem is, most of the obvious signs that things are going badly alert us rather late. By the time you start to see an increase in deaths or hospitalizations, the disease has already spread dramatically. Most of our solutions for controlling the disease spread include more testing — but, again, by the time someone seeks testing, they are already sick and have likely already infected many others.
The best approach would be to test everyone every day, but this is logistically and financially nearly impossible to achieve.
So we (along with others) were excited to see this paper back in June, which describes how to use sewage as a leading indicator for a SARS-CoV-2 outbreak (some of us were also excited at the opportunity to explain it to our five-year-olds). This was followed by the CDC and the US Department of Health and Human Services launching the National Wastewater Surveillance System. And most recently, University of Arizona researchers claimed that they used sewage detection to prevent an outbreak that could’ve been caused by two infected but unaware students in an on-campus dorm.
What’s the Basic Idea?
People who have COVID-19 shed the SARS-CoV-2 virus in their feces. Since viral replication and shedding typically begins before people feel sick (and certainly before they end up in the hospital), it is possible to detect the virus in the poop of infected individuals before symptoms show and patients seek care.
Doing this on an individual scale is probably not feasible — if we cannot get around to testing people with a nasal swab on a regular basis, it is hopeless to imagine reliably collecting everyone’s poop. But at a population level (or campus level), we might be able to use poop testing more effectively. That is, if you test a whole city or University’s poop at the same time, you might be able to detect that the virus is growing just a few days earlier than you would with, say, individual PCR test results.
There is some precedent for this type of fecal surveillance. It is used for polio screening, for example. In addition, the general idea of group or batch testing (where samples are pooled and then tested) is something that has been discussed in the context of non-fecal COVID-19 viral testing. Fecal screening, in a way, is kind of just large scale group testing.
What Do Researchers Do?
The concept is pretty simple: Researchers work with a sewage treatment plant to collect sewage and test it for SARS-CoV-2 viral particles. They can then compare the amount of SARS-CoV-2 virus in the sewage to hospital admission and case counts in the area, or to virus levels from a previous sample.
In the case at University of Arizona, researchers detected elevated levels of the virus coming from one dorm in particular. They tested all students living in the dorm, and found 2 asymptomatic individuals positive for COVID-19. These students were quarantined and contact tracing was used to track other possible infections.
What evidence do we have that this works?
The original paper researching SARS-Cov-2 presence in poop reported a time course of SARS-CoV-2 RNA concentrations in sewage in New Haven, Connecticut and compared it to a curve of COVID-19 hospitalization rates and infection rates detected by PCR testing. The researchers found that the trend for SARS-CoV-2 detected in poop mimics and leads the trend for hospitalization rates and case counts. Basically: poop is a leading indicator of SARS-CoV-2 infection.
The first plot below shows virus counts in poop (red) and hospitalizations (grey) by day. The lines are smoothed versions of the dots. In the second plot, we see only the lines. The two series seem to increase and decrease together. In the second plot you can see that the fecal virus counts peak just a bit before the hospitalizations peak. In fact, it’s about 3 days. (For the eagle eye reader: the scales change between the graphs since you need less range to look only at the smoothed lines).
Interestingly, if you look at COVID-19 case counts rather than hospitalizations, the fecal DNA leads by about a week. This means that fecal data allows us to react sooner than if we were only observing case counts or hospitalizations.
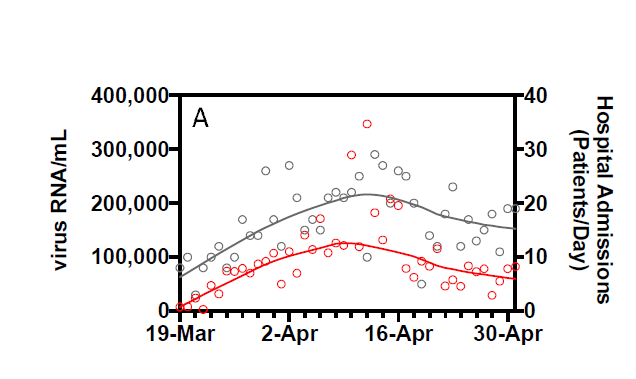
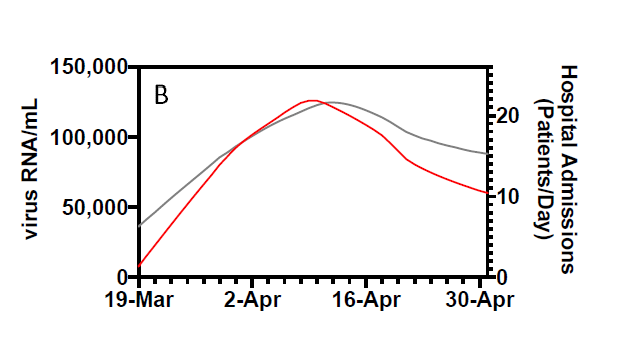
The researchers also took on the question of how correlated these series are. Correlations are measured from 0 to 1, where a value of 1 indicates perfect correlation (meaning the increase in concentration of virus particles in feces scales perfectly with the increase in COVID-related hospital admissions) and a value of 0 signifies no correlation (meaning there is no relationship between the concentration of virus particles in feces and the number of COVID-related hospital admissions). If you look at the lines only — that is, if you correlate the averaged data — the correlations are really, really high. The paper reports these smoothed lines have a correlation of 0.99.
Comments on the paper have pointed out that at the day to day level, correlation is lower, more like 0.5 (that is, if you look at the correlation in the dots rather than the lines). But this is still really high! Bottom line: virus in poop moves first.
How is this Being Used Today?
A research team at Yale believes that this method is giving them a better idea of viral spread in the New Haven. Each week, they report virus levels detected in sewage samples to the New Haven city officials. As New Haven starts to reopen, they expect to detect elevated levels of virus in the sewage, and this information will give the city an opportunity to act quicker than if they were depending on hospital data.
Carmel, Indiana has partnered with biotech company Biobot to collect and analyze the levels of virus in their wastewater. Mayor Jim Bainard says that if the sewage data shows a spike, he knows that they’ll need to draw back on some of their reopening.
Several universities in addition to University of Arizona, including Syracuse and University of California San Diego, are implementing sewage testing in an attempt to detect and halt potential outbreaks on campus.
Fecal sampling is unlikely to be our major viral detection tool: testing is still super important to identify infection on an individual level. However, as an addition to the slate of possible detection methods, it;s proved useful so far. Relative to doing medical testing on all individuals in the population, collecting poop from a vat is much, much easier.
